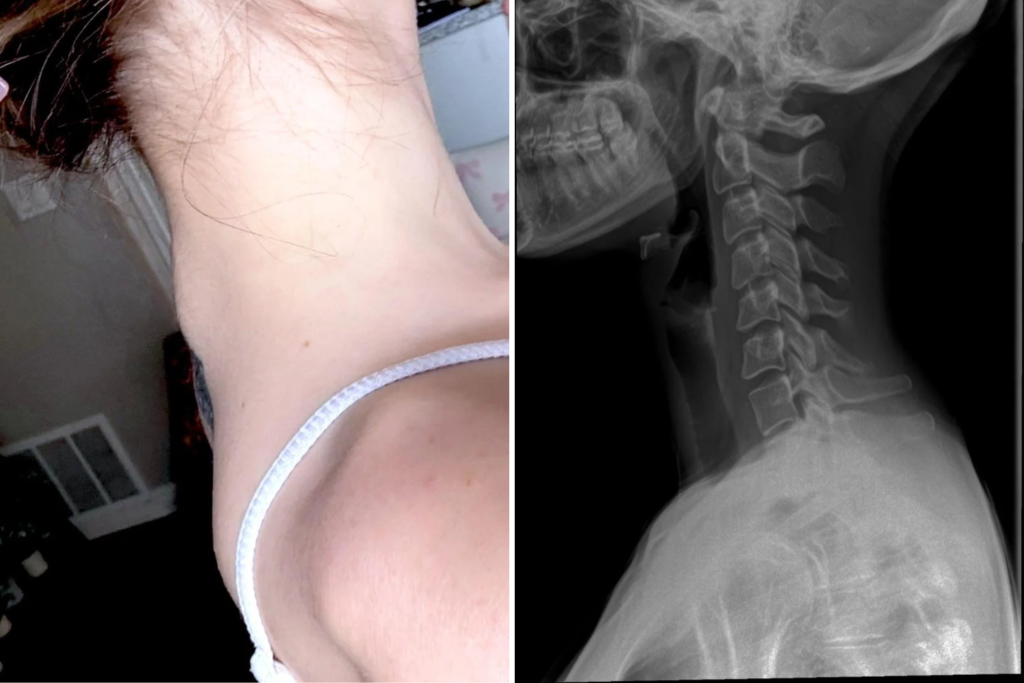
What started as a routine treatment for chronic migraines left 26-year-old Ty Jenkins with an unexpected side effect when her neck started to visibly curve outward.
Just days after a routine Botox injection to treat her migraines, Jenkins, who lives in Orange County, California, noticed something was wrong. “I started getting Botox in the summer of 2023 for migraines and TMJ,” she told Newsweek.
TMJ stands for temporomandibular joint, which connects the lower jaw to the temporal bones of the skull. These joints allow the jaw to move up and down, side to side, and forward and back, enabling essential functions such as chewing, talking, and yawning.
TMJ disorder, which is what Jenkins suffers with, is a group of conditions that cause pain and dysfunction in the jaw joint and surrounding muscles, potentially leading to pain, clicking, popping, or difficulty moving the jaw.
Botox is a brand name, but it has become widely used as a generic term for botulinum toxin type A injections in both medical and cosmetic contexts. Newsweek reached out to Botox’s parent company AbbVie, but a spokesperson did not have anything to add.
Migraines and TMJ disorders are often linked as they both involve the trigeminal nerve, which provides sensation to the face, jaw, and intracranial arteries.
Jenkins had Botox in her face and the back and sides of her head, in her shoulders, and in her neck. She said that the treatment did help with her TMJ and migraines. But, after her most-recent treatment on March 13, things changed rapidly.
“The last two appointments [they have] been putting more in my neck. I first noticed the bump a little over a week later—it developed fully over just a matter of days,” Jenkins said. “I know my neck and back very well … I noticed right away when something was different.”
Initially hesitant due to past medical experiences, Jenkins waited a few days before seeing her general practitioner, who ordered X-rays and referred her to a rheumatologist. The specialist quickly suspected hypermobile Ehlers-Danlos syndrome (hEDS) and craniocervical instability (CCI)—two rare connective tissue disorders.
Ehlers-Danlos syndrome (EDS) is an inherited group of disorders that affect connective tissues, especially the skin, joints and blood vessel walls. People with EDS often experience extremely flexible joints and stretchy, fragile skin. CCI is a structural disorder characterized by excessive movement between the skull and the upper cervical spine (C1-C2 vertebrae).
“[The specialist] believes I have both,” Jenkins said, though she is now awaiting further evaluation at a specialized EDS clinic.
Jenkins said that her doctor believes Botox may have unintentionally triggered the visible spinal change by relaxing muscles that were compensating for already-loose ligaments in her neck. This led to a rapid shift in posture and a cascade of worsening symptoms including intensified pain, headaches, and vision issues.
Jenkins’s rheumatologist has since advised her to stop getting Botox in the neck, at least until she sees a spine specialist.
Dr. Steven A. Hanna, a Royal College-certified plastic surgeon, told Newsweek: “Botox can be very effective at reducing muscle-related tension and pain. That said, in patients with connective tissue disorders—like hypermobile Ehlers-Danlos syndrome or craniocervical instability—there’s a concern that relaxing stabilizing muscles in the neck may worsen preexisting instability.”
Jenkins shared her story on Reddit’s r/Wellthatsucks subreddit where it has prompted reaction from people online. In the post, she said: “The bones in my neck curved outward shortly after getting Botox for migraines, turns out my whole spine is a mess …”
In cases like Jenkins’, what may look like a Botox complication could actually be the “unmasking of an undiagnosed condition,” Hanna said. Muscles that have long been compensating for structural weakness can become less supportive, triggering noticeable deformities or worsening symptoms.
“Proper technique is also crucial,” Hanna added, emphasizing that misdirected injections in sensitive areas such as the neck could contribute to issues ranging from head drop to trouble swallowing.
As she awaits further diagnostic confirmation, Jenkins is sharing her story not to deter others from seeking relief, but to raise awareness of rare conditions that might otherwise go unnoticed. “If people have concerns, they should bring them up with their doctor and ask about craniocervical instability,” she said. “If they have CCI or EDS, they should definitely disclose that and consult an EDS specialist first.”
Read the full article here