The evolutionary trick of parasitic worm that sneakily burrows into the skin of its victims could provide new alternatives to opioid-based pain treatments.
Opioids are currently used to treat moderate to severe pain, as well coughing and diarrhea. Although they can provide effective relief, long-term use can also lead to dependence, with negative physical and mental health consequences.
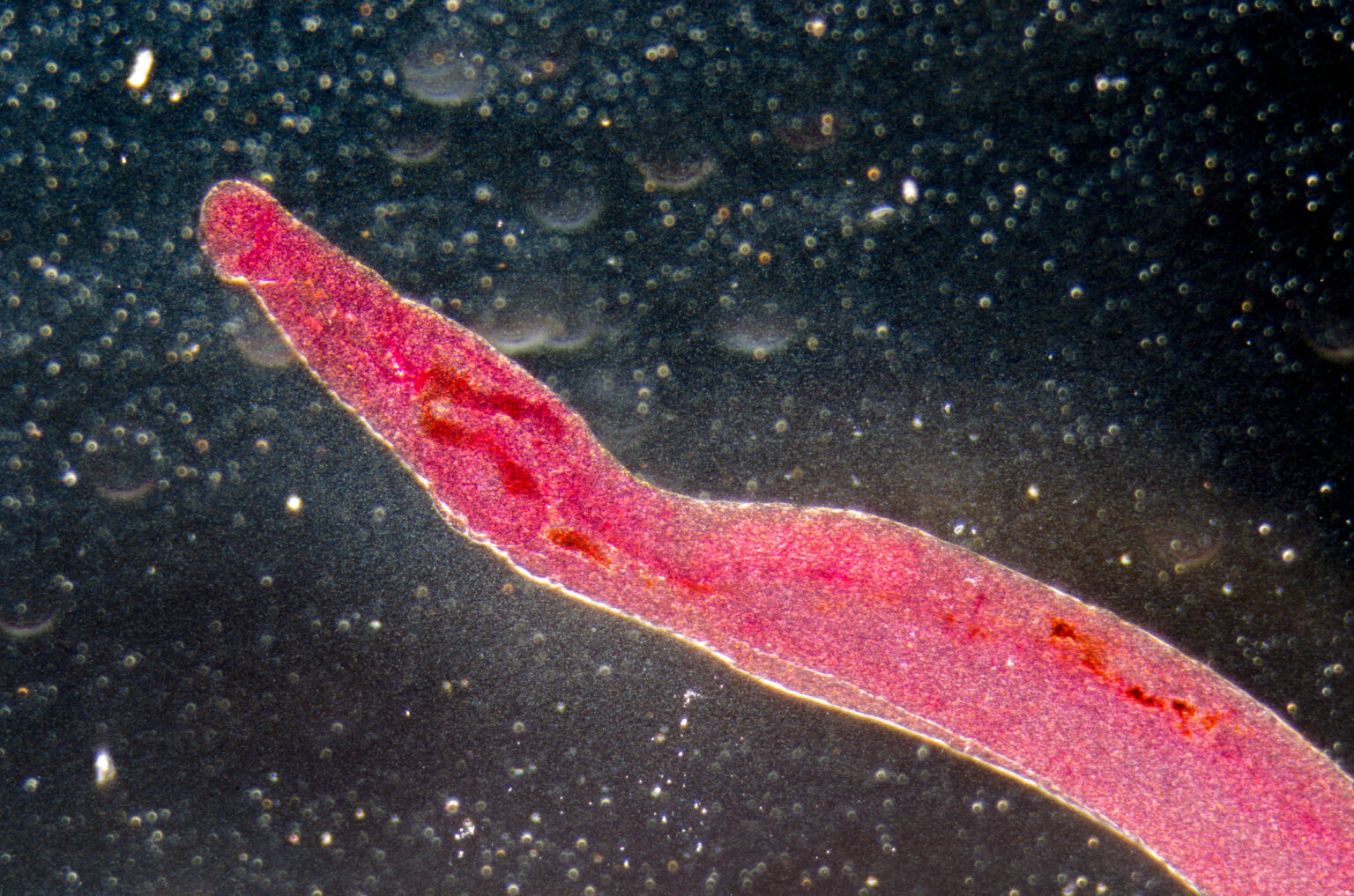
Researchers discovered that the worm—Schistosoma mansoni—suppresses neurons in the skin to evade detection in a mechanism likely developed to enhance its own survival.
The molecules responsible for this suppression of sensation could help in the development of new painkillers, according to the team at the Tulane School of Medicine.
Schistosomiasis is a parasitic infection caused by helminths, a type of worm known to survive in their mammal hosts for many years. Their larvae can infest freshwater bodies like lakes, ponds and rivers—infecting people who, for example, swim, fish or wash clothes in the water.
“While bacteria often cause painful cutaneous reactions, host skin invasion by the human parasitic helminth Schistosoma mansoni often goes unnoticed,” the researchers wrote in their paper.
S. mansoni often evades detection by the immune system, unlike other bacteria or parasites that cause pain, itching or rashes—a feat the team set out to investigate.
After conducting experiments on mice, the researchers found that S. mansoni produces molecules that suppress the activity of TRPV1+, a protein used to send signals that the brain interprets as heat, itching or pain.
As part of the pain-sensing process in sensory neurons, TRPV1+ regulates immune responses in scenarios including allergy, autoimmunity, cancer, infection and even hair growth, the researchers explained.
It is likely the parasitic worm evolved its ability to block TRPV1+ because it enhance its survival, the researchers said.
“If we identify and isolate the molecules used by helminths to block TRPV1+ activation, it may present a novel alternative to current opioid-based treatments for reducing pain,” said paper author and immunologist professor De’Broski R. Herbert| in a statement.
“The molecules that block TRPV1+ could also be developed into therapeutics that reduce disease severity for individuals suffering from painful inflammatory conditions.”
The study also revealed that TRPV1+ is necessary for initiating host protection against S. mansoni. Activation of the protein leads to rapid mobilization of immune cells, including gd T cells, monocytes and neutrophils, which induce inflammation.
This inflammation, the researchers explained, plays a crucial role in host resistance to the larval entry into the skin.
These findings highlight the importance of neurons that sense pain and itching in successful immune responses.
“Identifying the molecules in S. mansoni that block TRPV1+ could inform preventive treatments for schistosomiasis. We envision a topical agent which activates TRPV1+ to prevent infection from contaminated water for individuals at risk of acquiring S. mansoni,” said Herbert.
In the study, mice were infected with S. mansoni and evaluated for their sensitivity to pain as well as the role of TRPV1+ in preventing infection.
“S. mansoni infection significantly reduced thermal pain sensitivity evoked by TRPV1+ neurons. Consistently, isolated skin sensory neurons from infected mice had significantly reduced calcium influx and neuropeptide [chemical messenger] release in response to the TRPV1 agonist capsaicin [an irritant for humans and mammals] compared to neurons from naïve controls,” the study authors wrote.
“Using gain-and loss-of-function approaches to test whether TRPV1+ neurons initiate host-protective responses revealed that TRPV1+ neurons limit S. mansoni skin entry and migration into the pulmonary tract.”
The researchers are now planning to identify the nature of the secreted or surface-associated helminth molecules that are responsible for blocking TRPV1+ activity and specific gd T cell subsets that are responsible for immune responses. They also seek to further understand the neurons that helminths have evolved to suppress.
Newsweek has reached out to the researchers for additional comment.
Do you have a tip on a health story that Newsweek should be covering? Do you have a question about opioids? Let us know via health@newsweek.com.
Reference
Inclan-Rico, J. M., Stephenson, A., Napuri, C. M., Rossi, H. L., Hung, L.-Y., Pastore, C. F., Luo, W., & Herbert, D. R. (2025). TRPV1+ neurons promote cutaneous immunity against Schistosoma mansoni. The Journal of Immunology. https://doi.org/10.1093/jimmun/vkaf141
Read the full article here